Agentic AI in Blood Cancers: From First Clues to Personalized Treatment - and Back to Life

The moment a routine blood test blinks red, life tilts, within hours, you might hear about smear reviews, flow cytometry, bone marrow biopsies, and genomic sequencing followed by decisions about chemotherapy, targeted pills, or Chimeric Antigen Receptor T-cell therapy (CAR-T) and then the long vigil against relapse. In that whirlwind, imagine a steady supporting friend, a co-pilot. Agentic AI doesn't just make predictions, it plans, summons the right tools, and coordinates next steps. Used well, it helps clinicians move faster and more safely, and it makes care feel more personal. The payoff isn't only better medicine, it's more of what matters the most, time, clarity, and hope.
Agentic AI is different from the "assistive" AI you may have heard about. Traditional systems offer a single prediction ("this looks suspicious"); a clinician takes it from there. Agentic AI goes further. It can break a complex goal into steps, choose and use the right resources (imaging, guidelines, trusted knowledge bases), double-check its own work, and hand a clear decision-support package to a clinician for sign-off. Think of it as a careful, supervised teammate that can plan and act but always with a human in the loop.
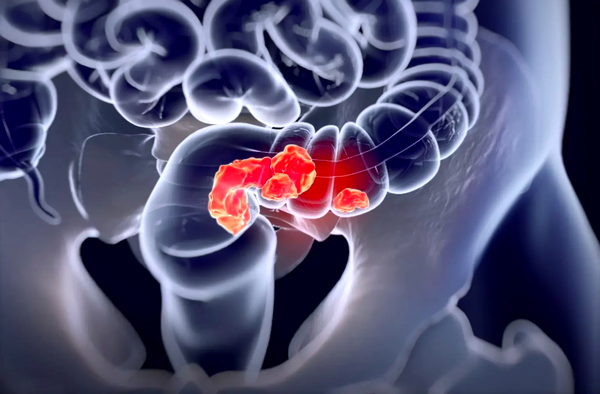
Getting to the right diagnosis sooner
Early on, speed and accuracy matter. Modern “digital hematology” tools can scan blood smears the thin layers of blood spread on a glass slide and highlight unusual cells for urgent review. In the pathology lab, whole-slide images of tissue are large and complex. AI can help spot patterns and suggest what to look at first. These tools don’t replace specialists, but they help standardize the steps, reduce delays, and document how a conclusion was reached. That’s exactly where agentic AI shines, it can route the right images to the right expert, attach the right references, and keep an audit trail so every step is transparent.
From DNA findings to real options
When genetic testing (sequencing) returns, the hard part is turning variants, tiny changes in DNA into actionable insights. Agentic AI can read the lab report, look up what each variant means in vetted knowledge bases (for example, whether a change is tied to an approved treatment or a clinical trial), and present the care team with a short, plain-language summary: what was found, why it matters, and what to consider next. In practice, that might mean flagging a targetable mutation, listing standard-of-care options, and suggesting a few nearby trials that truly fit the patient’s situation. Every source is cited in the background, so clinicians can check the evidence quickly.
Tailoring therapy to this patient
Blood cancers are not one-size-fits-all. Risk depends on age, the behaviour of the disease, and which genetic changes are present. Rather than relying only on broad categories, agentic systems can synthesize many details at once to estimate the chances of remission or relapse and to suggest the intensity of treatment. That can help teams time decisions like whether to consider a stem-cell transplant early, or whether a targeted drug should be added to chemotherapy.
Choosing (and sequencing) the right therapies
Once a patient’s tumor DNA has been analyzed and each variant is annotated (labeled with its meaning), the agent can map those findings to a trusted guidelines and scan for active clinical trials that truly match the patient’s profile. Some platforms already match genomic data to trial criteria, but newer, language-model–powered systems go further, they read the free-text details in trial listings and the unstructured notes in an electronic health record, then line them up. The result is a short, clear list of options, each with a simple “why this fits” delivered to the care team without hours of manual searching.
Here's what that feels like in real life: suppose a report shows a mutation in a gene that makes a receptor an "on/off switch" on early blood-forming cells (FLT3 which is often called CD135) in the bone marrow. In certain leukemias, that switch can get stuck "on." The agent highlights guideline-supported treatments for FLT3-positive disease and instantly filters hundreds of trials down to a handful that accept adults with this exact mutation, the right prior treatments, and no conflicting conditions. That saves staff time, speed decisions, and opens doors patients might otherwise miss.
Seeing side effects before they hit
Chimeric Antigen Receptor T-cell therapy (CAR-T) has changed the outlook for some relapsed leukemias, lymphomas, and myeloma. But it can cause serious inflammatory side effects, such as cytokine release syndrome (CRS) or temporary neurologic symptoms. Agentic AI can continuously watch vital signs, lab trends, and patient-reported symptoms. If a risk score crosses a threshold, it alerts the care team and recommends the next step based on protocol, sometimes hours before a person feels worse. In the background, it keeps everything documented, what triggered the alert, who responded, and how the person did afterward.
Guiding recovery and the long road back
Finishing treatment isn’t the finish line, it’s the start of follow-up. Many blood cancers are now monitored with MRD tests (measurable/minimal residual disease), which can detect tiny amounts of cancer that ordinary tests might miss. Agentic AI can track MRD results over time, line them up with scans and routine labs, and recommend guideline-aligned next steps when something changes like repeating a test sooner, adjusting therapy, or booking a specific clinic visit.
Care doesn't stop at the clinic door, either. Simple weekly check-ins called ePROs, or electronic patient-reported outcomes let people report symptoms at home. When done well, these check-ins can reduce emergency visits and improve quality of life. An agent can schedule messages around chemo cycles, nudge gently when someone forgets to respond, and escalate red-flag symptoms to the on-call team with the right context. It can also help build a survivorship plan that covers vaccines, bone health, fertility, and long-term screening and then keep the plan on track.
What “good” looks like: safety, fairness, and fit-for-purpose
Good systems put humans firmly in the loop. Agents recommend and coordinate; clinicians approve and explain. They are built on evidence and transparency, validated across multiple hospitals, with clear uncertainty reporting and checks for bias. From day one, they align with standards and regulation (for example, clear change-control plans and transparency principles) so updates are safe and traceable. And they protect privacy and equity, trained and tested on diverse data, decisions logged for audit, and patient-facing explanations written in plain language and available in multiple languages.
A realistic blueprint for an agentic hematology co-pilot
The journey starts at intake and triage level. The system notices abnormal blood counts, pulls relevant prior results, and kicks off the smear-review workflow. If blast counts or other red flags exceed a threshold, it alerts the hematology team with a brief rationale, so the right person acts quickly.
Next comes a diagnostic pack. The agent links AI readouts from smear, flow cytometry, and pathology with radiology findings and the first wave of genetic data, then drafts a structured note, the leading possibilities, what evidence supports them, and what to confirm next.
From genomics to options, the agent annotates variants with evidence levels, lines them up with standard-of-care therapies, compassionate-use possibilities, and suitable clinical trials, and even pre-populate consent and medical aid (insurance) forms to reduce delays.
During treatment, safety is continuous. The system monitors vitals, labs, and patient-reported symptoms, runs CRS risk checks after CAR-T when relevant, and escalates to the care team according to protocol when thresholds are met.
Finally, recovery and survivorship are planned, not improvised. The agent tracks Minimal / Measurable Residual Disease (MRD), vaccination status, bone health, fertility considerations, and late-effects screening. When anything drifts from plan, it messages the team with context and suggests next steps.
What’s coming next
First, expect multimodal “foundation” agents systems that can reason across text, images, and time-series data, then act. Early deployments will be tightly scoped and auditable, with safety checks built in. Second, trial access will get smarter and faster. Language-model matchers that read free-text eligibility and real-world notes promise broader enrollment, especially for rare subtypes that often slip through manual screens. Finally, we’ll see learning health loops. As MRD results, home-reported symptoms, and side-effect data stream in, agents can learn which sequences of care truly change outcomes and feed those insights back into practice under appropriate oversight.
So where should teams begin?
Start where the evidence is strongest: AI assists in smear and pathology, variant annotation with trusted knowledge bases, ePRO monitoring, smart trial matching, and MRD-aware follow-up. Wrap every step in governance, human sign-off, audit logs, bias checks, and clear, regulator-aligned change-control and transparency. Above all, treat agentic AI as a workflow teammate that augments clinicians, not a black-box oracle.